Complaint Handling: Understanding Grievance Mechanism Procedures
- Jun 4, 2025
- 5 min read

An aggrieved patient may pursue a medical negligence claim when their complaint relates to the standard of clinical care they received and it is alleged that this care fell below an acceptable standard. However, not all patient grievances amount to a medical negligence claim. In some cases, dissatisfaction may stem from the conduct or attitude of a medical practitioner, healthcare worker or other staff members at a private healthcare facility. A patient may also be aggrieved by non-clinical matters such as billing disputes or administrative shortcomings.
Broadly speaking, patients may raise grievances relating either to clinical care or to non-medical issues and it is important to understand the appropriate channels and thresholds applicable to each type of complaint.
Complaints To The Ministry of Health, Malaysia
Against Government Healthcare Facilities
The Corporate Communications Unit (UKK) is the front-line unit of the Ministry of Health (MOH) where it has established a complaints mechanism for patients to lodge a complaint or grievance relating to events that occurred in a government healthcare facility.
Meanwhile, Sistem Pengurusan Aduan Awam (SisPAA) is an online channel to manage feedback such as complaints, appreciation, inquiries and suggestions from the public regarding MOH services. Complaints made can relate to:
o delayed treatment
o failure to follow standard operating procedures
o misconduct
o shortage of facilities
o overall unsatisfactory quality of service provided
The timeframe for resolving complaints is typically 15 working days. However, in cases involving complex issues, the resolution period may extend from 16 up to 365 days, depending on the nature and severity of the complaint.
Against Private Healthcare Facilities
Complaints against a private healthcare facility fall within the purview of the Private Medical Practice Control Section (CKAPS), a unit under the Medical Practice Division of the MOH. A complaint may be lodged with CKAPS in writing via email, by letter or in person.
CKAPS serves as the regulatory authority responsible for monitoring, enforcing and ensuring compliance with the Private Healthcare Facilities and Services Act 1998 (PHFSA) and its subsidiary regulations. Complaints made to CKAPS typically concern breaches by private healthcare facilities such as excessive or unauthorised charges, or failure to meet prescribed statutory standards.
It should be noted, however, that if the complaint pertains specifically to the conduct or clinical practice of a medical practitioner within a private healthcare facility, CKAPS may not be the appropriate forum for redress. In such instances, alternative channels, such as the Malaysian Medical Council, may be more suitable.
Complaints To A Private Healthcare Facility/ Private Medical Or Dental Clinic
When a grievance is raised, whether made verbally or in writing, the healthcare facility or clinic will need to conduct an investigation and provide a written reply to the complainant. All complaints must be documents and any report generated in the course of investigation may be discoverable in court.
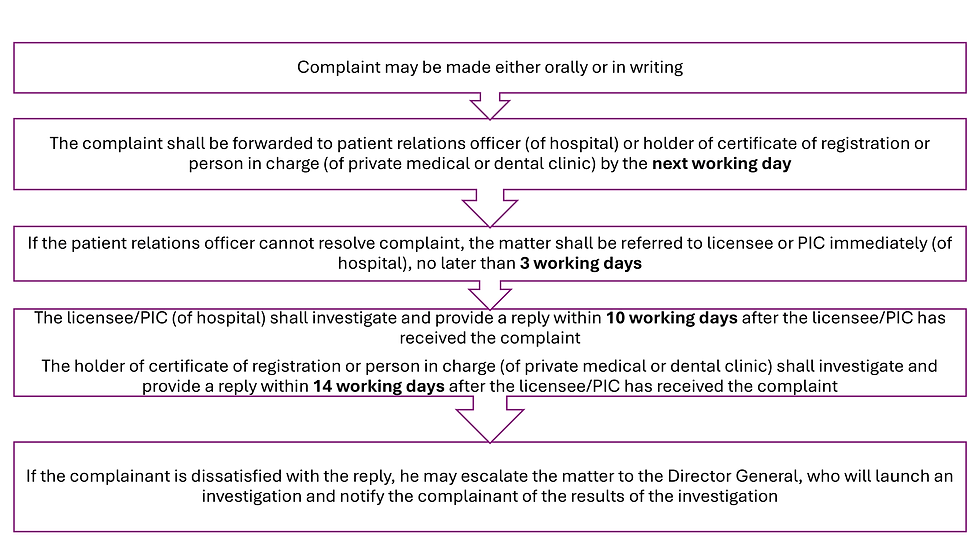
There exists a statutory framework governing grievance procedures within private healthcare facilities and private medical and dental clinics. For private healthcare facilities, this framework is prescribed under Regulation 40 of the Private Healthcare Facilities and Services (Private Hospitals and Other Private Healthcare Facilities) Regulations 2006. For private clinics and dental clinics, the applicable provision is Regulation 27 of the Private Healthcare Facilities and Services (Private Clinics or Private Dental Clinics) Regulations 2006.
The grievance procedure is generally structured as follows:
Complaints To The Malaysian Medical Council
The Malaysian Medical Council (MMC) is the statutory body responsible for regulating all registered medical practitioners in Malaysia, encompassing both those in private
practice and those serving in the government sector. The MMC exercises disciplinary jurisdiction over practitioners through the conduct of formal inquiries in accordance with its regulatory functions.
The MMC’s powers to impose disciplinary sanctions are derived from the Medical Act 1971. It is important to note, however, that the MMC’s jurisdiction is generally limited to matters involving ethical or professional misconduct.
MMC’s disciplinary jurisdiction
The MMC enforces the ethical codes and guidelines it issues through the exercise of its disciplinary jurisdiction under Section 29 of the Medical Act 1971. Where a registered medical practitioner is found to have breached professional or ethical standards, the Council is empowered, pursuant to Section 30 of the Act, to impose any of the following disciplinary sanctions:
(a) reprimand the medical practitioner;
(b) order such medical practitioner’s registration to be subjected to conditions which may include but are not limited to one or more of the following:
(i) that the medical practitioner seek medical treatment;
(ii) that such conditions relating to the medical practitioner’s practice of medicine as it considers appropriate be imposed on the medical practitioner’s registration;
(iii) that the medical practitioner undergo educational courses or programmes as may be specified by the Council; or
(iv) that the medical practitioner report on his medical practice to such medical practitioner or persons as may be specified by the Council;
(c) order the name of such medical practitioner to be suspended from the Register for such period as it thinks fit;
(d) make such order in paragraph (c) but suspend the application thereof, subject to such conditions as the Council may think fit, for a period, or periods in the aggregate, not exceeding two years; or
(e) order the name of such medical practitioner to be struck off the Register.
Appeal Against MMC’s Disciplinary Decision
Section 31 of the Medical Act 1971 provides for a statutory right of appeal to the High Court against any order made by the MMC in the exercise of its disciplinary jurisdiction. An appeal is filed by way of originating summons within one month of the MMC’s order.
Section 31(1) reads as follows:
“Any person who is aggrieved by any order made in respect of him by the Council in the exercise of its disciplinary jurisdiction may appeal to the High Court, and the High Court may thereupon affirm, reverse or vary the order
appealed against or may give such direction in the matter as it thinks proper; the cost of the appeal shall be in the discretion of the High Court.”
From the wordings of this provision, the right to appeal only applies to those who are aggrieved by the order made in respect of him. Therefore, a complainant cannot appeal to the High Court following any decision by the MMC to dismiss the complaint made against a medical practitioner. The only option left would be to seek judicial review of the MMC’s decision, subject to obtaining leave of the Court.
Commentary
Ultimately, ensuring that grievances are directed to the correct forum enhances the likelihood of a meaningful resolution and upholds both the integrity of the healthcare system and public trust in it.
It bears emphasising that the manner in which a complaint is received and handled, whether in a private or government healthcare setting, can significantly influence whether the matter is resolved amicably or escalates further. Grievances should be approached with care, transparency and professionalism. A prompt and respectful response not only demonstrates accountability but may also prevent a dissatisfied patient from pursuing formal legal action or regulatory complaints.
4 June 2025



